Welcome to this informative article on how dry eye severity is diagnosed and evaluated! If you’ve been experiencing symptoms such as itching, burning, or redness in your eyes, it’s important to understand how healthcare professionals assess the severity of your condition. By understanding the diagnostic process, you can work with your healthcare provider to find the right treatment plan to help you find relief from dry eye symptoms. Let’s explore the different methods used to evaluate the severity of dry eye and how you can take steps to improve your eye health. How Is Dry Eye Severity Diagnosed And Evaluated?
Hey there! Have you been experiencing dry, itchy, or irritated eyes lately? It’s essential to understand how dry eye severity is diagnosed and evaluated to receive proper treatment and relief. Let’s dive into the different methods and tools used by eye care professionals to assess the severity of dry eye syndrome.
Symptoms of Dry Eye
Dry eye syndrome can manifest in various symptoms that can affect your daily life. Common symptoms include itching, burning, redness, and a gritty sensation in the eyes. You may also experience excessive tearing as your eyes try to compensate for the lack of moisture. If you have been experiencing any of these symptoms, it’s essential to seek assistance from an eye care professional for proper diagnosis and treatment.
How to Recognize Dry Eye Symptoms
If you find yourself constantly reaching for eye drops or experiencing discomfort, you may be suffering from dry eye syndrome. Other signs to watch out for include blurry vision, sensitivity to light, and the feeling of something in your eye. Pay attention to how your eyes feel throughout the day and keep track of any symptoms you may be experiencing to discuss with your eye care provider.
Diagnostic Tests for Dry Eye
When you visit an eye care professional for evaluation, they will perform several diagnostic tests to determine the severity of your dry eye syndrome. These tests help identify the underlying causes of your symptoms and guide your treatment plan. Let’s explore some of the common diagnostic tests used for assessing dry eye severity.
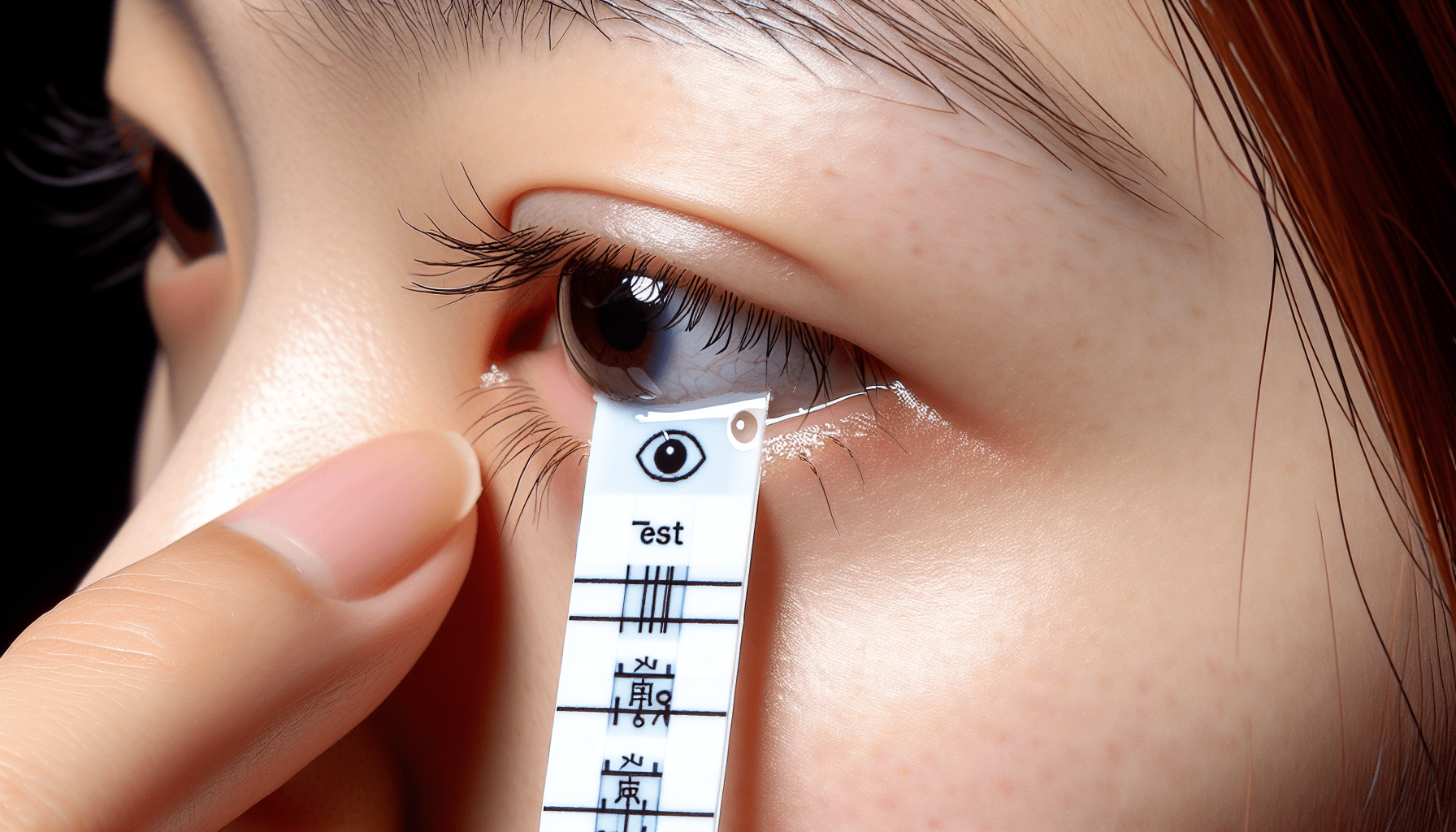
Schirmer’s Test
One of the most common diagnostic tests for dry eye is the Schirmer’s test. This test measures the production of tears by placing a thin strip of specialized paper under your lower eyelid. The amount of moisture absorbed by the paper over a few minutes indicates the level of tear production, helping your eye care provider assess the severity of your dry eye syndrome.
Tear Break-Up Time (TBUT) Test
The Tear Break-Up Time (TBUT) test evaluates the stability of the tear film on the surface of your eye. During this test, a special dye is placed in your eye, and your eye care provider observes how long it takes for your tears to break up or evaporate. A shorter break-up time indicates instability in the tear film, contributing to dry eye symptoms.
Osmolarity Test
The Osmolarity test measures the concentration of salt and other particles in your tears. High osmolarity levels can indicate inflammation and damage to the eye’s surface, contributing to dry eye symptoms. By evaluating the osmolarity of your tears, your eye care provider can assess the severity of dry eye syndrome and tailor your treatment plan accordingly.
Evaluating Dry Eye Severity
After performing diagnostic tests to identify the root cause of your dry eye symptoms, your eye care provider will evaluate the severity of your condition. Understanding the severity of dry eye syndrome is crucial for developing an effective treatment plan that addresses your unique needs. Let’s explore how dry eye severity is assessed by eye care professionals.
Grading Dry Eye Severity
Dry eye severity is often classified into different grades based on the frequency and intensity of symptoms, as well as the results of diagnostic tests. The following grading system is commonly used to assess the severity of dry eye syndrome:
- Grade 1: Mild dry eye, minimal symptoms with occasional discomfort
- Grade 2: Moderate dry eye, frequent symptoms that impact daily activities
- Grade 3: Severe dry eye, constant discomfort affecting quality of life
- Grade 4: Very severe dry eye, debilitating symptoms requiring immediate treatment
By assigning a grade to your dry eye severity, your eye care provider can determine the appropriate treatment options and monitor your progress over time.
Meibomian Gland Dysfunction (MGD)
Meibomian Gland Dysfunction (MGD) is a common underlying cause of dry eye syndrome, especially in patients with evaporative dry eye. Your eye care provider may evaluate the function of your meibomian glands, which produce the oily layer of the tear film. Dysfunction in these glands can lead to tear film instability and dry eye symptoms, requiring specific treatment approaches to address the root cause of your condition.
Inflammation and Demodex
Inflammation and infestations of Demodex mites on the eyelids can contribute to dry eye severity and discomfort. Your eye care provider may perform additional tests to assess the presence of inflammation or Demodex infestations, guiding targeted treatment options to alleviate your symptoms. Addressing underlying inflammation and infestations is essential for managing dry eye syndrome effectively.
Tailoring Treatment Plans
Once the severity of your dry eye syndrome has been evaluated, your eye care provider will work with you to develop a customized treatment plan that addresses your specific needs and symptoms. Treatment options may vary based on the underlying causes of your dry eye severity and the grade of your condition. Let’s explore some common treatment approaches for managing dry eye syndrome.
Artificial Tears
Artificial tears are a popular treatment option for mild to moderate dry eye symptoms. These lubricating eye drops help moisturize the surface of your eyes, providing relief from dryness and irritation. Your eye care provider may recommend specific types of artificial tears based on the severity of your condition and your individual needs.
Prescription Eye Drops
For more severe cases of dry eye syndrome, prescription eye drops may be necessary to manage inflammation and promote tear production. Anti-inflammatory eye drops and medications that stimulate tear production can be prescribed by your eye care provider to address underlying causes of dry eye severity and alleviate symptoms.
Warm Compresses and Lid Hygiene
Meibomian Gland Dysfunction (MGD) can benefit from warm compresses and lid hygiene practices to improve the function of the oil-producing glands in your eyelids. By applying warm compresses and gently cleaning your eyelids, you can alleviate blockages in the glands and promote a healthier tear film, reducing dry eye severity and discomfort.
Punctal Plugs
Punctal plugs are small devices inserted into the tear ducts to block the drainage of tears, keeping the eyes moist and lubricated. This treatment option is beneficial for patients with severe dry eye syndrome who struggle with inadequate tear production. Your eye care provider can determine if punctal plugs are suitable for managing your dry eye severity.
Lifestyle Modifications
Making lifestyle changes can also help manage dry eye severity and improve the quality of your tears. Stay hydrated, avoid excessive screen time, protect your eyes from environmental factors, and incorporate omega-3 fatty acids into your diet to support tear production and alleviate dry eye symptoms. Your eye care provider can provide personalized recommendations for lifestyle modifications based on your specific needs.
Follow-Up Care and Monitoring
After initiating a treatment plan for managing your dry eye severity, it’s essential to follow up with your eye care provider for ongoing monitoring and adjustments. Regular check-ups allow your provider to assess your progress, make any necessary changes to your treatment plan, and address any new symptoms or concerns that may arise. By staying engaged in your eye care and communicating openly with your provider, you can achieve improved eye health and greater comfort.
Importance of Communication
Remember that open communication with your eye care provider is key to effectively managing dry eye severity. Be sure to discuss any changes in your symptoms, concerns about your treatment plan, or new issues that may impact your eye health. Your provider is there to support you and guide you on the journey to healthier, more comfortable eyes.
Benefits of Routine Eye Exams
Regular eye exams are essential for monitoring your eye health and catching any potential issues early on. By scheduling routine visits with your eye care provider, you can stay proactive in managing dry eye severity and addressing any other concerns related to your eye health. Don’t wait until symptoms worsen – prioritize your eye care and well-being by staying on top of your eye exams.
In conclusion, understanding how dry eye severity is diagnosed and evaluated is crucial for receiving proper treatment and relief from symptoms. By recognizing common symptoms, undergoing diagnostic tests, assessing the severity of your condition, and developing a tailored treatment plan, you can effectively manage dry eye syndrome and improve your eye health. Remember to stay engaged in your eye care, communicate openly with your provider, and prioritize routine monitoring to achieve optimal outcomes. Take charge of your eye health, and let your eyes shine bright with comfort and clarity.