Have you ever wondered why you feel weak when you’re sick? It turns out that your immune system plays a crucial role in these feelings of weakness. When your body detects an illness or infection, your immune system kicks into high gear to fight off the invaders. But this immune response can also lead to the release of certain chemicals that make you feel tired and sluggish. In this article, we’ll explore how the immune system contributes to these feelings of weakness and what you can do to support your body during times of illness. Get ready to uncover the fascinating connection between your immune system and those dreaded feelings of fatigue!
Overview of the Immune System
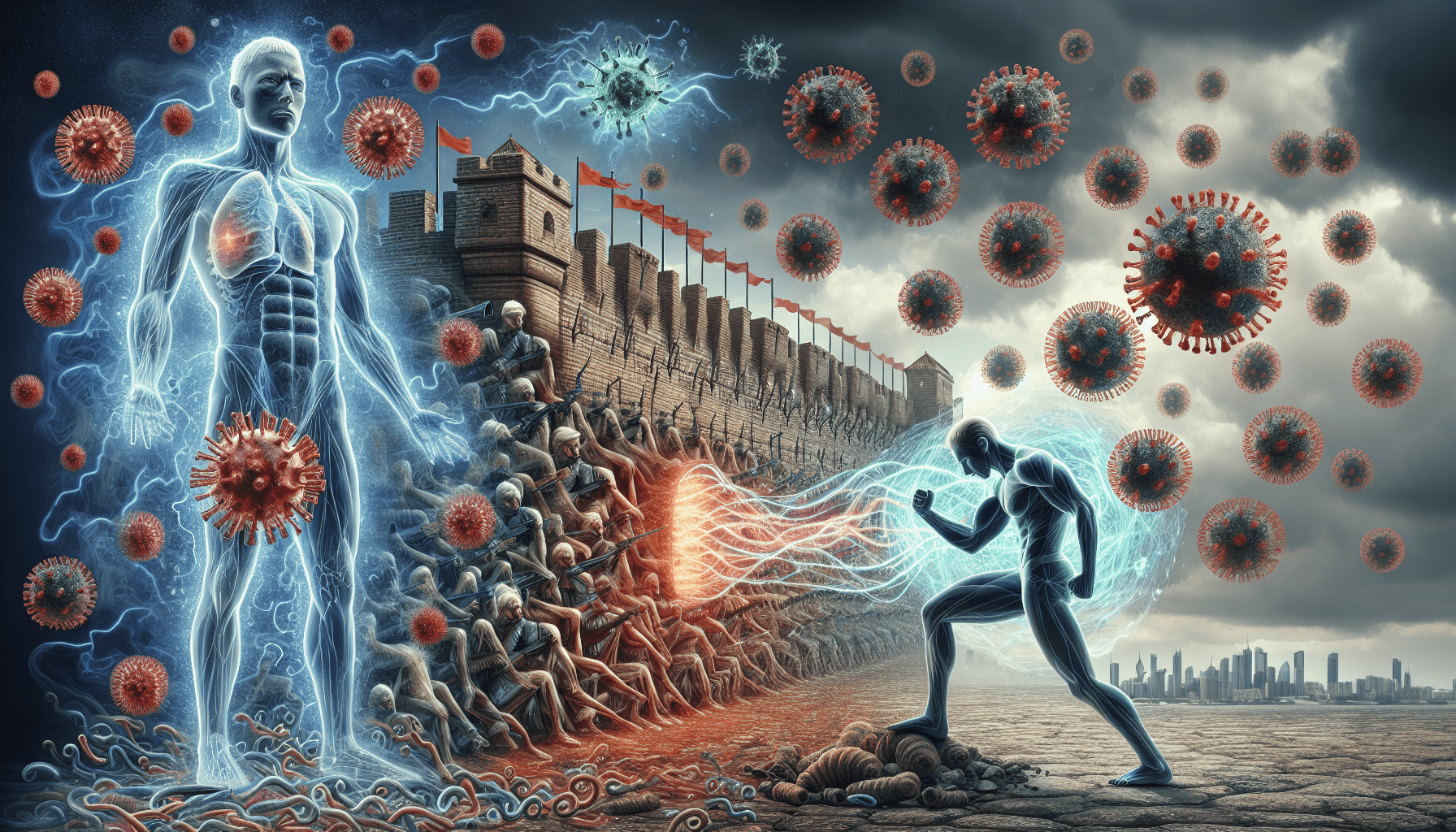
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful pathogens, such as bacteria, viruses, and parasites. Its primary function is to identify and eliminate these invaders while maintaining the body’s overall health. Without a properly functioning immune system, the body becomes vulnerable to infections and diseases.
The immune system is made up of various components, including white blood cells, antibodies, lymph nodes, and the thymus gland. These components work harmoniously to recognize and respond to foreign substances, known as antigens. The immune system’s intricate mechanisms ensure a swift and effective defense against pathogens.
Immune Response to Pathogens
When a pathogen enters the body, the immune system kicks into action to recognize and combat the invader. The first step in this process is the recognition of antigens by immune cells. Specialized receptors on the surface of these cells identify specific antigens and trigger an immune response.
Once the antigens are recognized, immune cells, such as macrophages and dendritic cells, become activated. They engulf and destroy the pathogens, preventing their further spread in the body. Additionally, these activated cells release inflammatory substances, such as cytokines and chemokines, which attract other immune cells to the site of infection.
Inflammatory Response
Inflammation is a vital component of the immune response, as it helps to eliminate pathogens and initiate the healing process. When immune cells release inflammatory substances, blood vessels in the affected area dilate, allowing more immune cells and nutrients to reach the site of infection. This increased blood flow leads to redness, swelling, and warmth, which are common symptoms of inflammation.
The inflammatory response also triggers the activation of more immune cells, such as neutrophils and natural killer cells, which further aid in pathogen eradication. However, inflammation can sometimes become chronic, leading to long-term tissue damage and the development of inflammatory diseases.
Interplay between the Immune System and Energy
The immune response requires a substantial amount of energy to mount an effective defense against pathogens. During an infection, the body increases its metabolic rate to support immune cell activation, proliferation, and the production of antibodies. This increased energy expenditure can lead to feelings of fatigue and exhaustion.
Moreover, the immune response can impact energy balance by altering appetite and metabolism. Inflammatory substances released during immune activation can suppress appetite, leading to reduced food intake. Additionally, the body may shift its energy utilization towards supporting the immune system, which can further contribute to feelings of weakness.
The immune system also plays a crucial role in controlling metabolism. It regulates insulin sensitivity, glucose metabolism, and lipid metabolism, ensuring a balanced energy utilization. Disruptions in immune function, such as in autoimmune diseases, can lead to metabolic dysregulation and subsequent weakness.
Cytokines and Fatigue
Cytokines are small proteins produced by immune cells that act as messengers between cells, facilitating communication during immune responses. Different types of cytokines have distinct effects on the body. For example, pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha), promote inflammation and can induce feelings of weakness and fatigue.
These cytokines can directly affect the nervous system, altering neurotransmitter levels and disrupting the normal functioning of the brain. They can also have indirect effects on muscle function and contribute to muscle fatigue. The release of pro-inflammatory cytokines during immune activation can therefore lead to the overall sensation of weakness throughout the body.
Immune System Disorders and Weakness
Several immune system disorders can contribute to feelings of weakness. Autoimmune diseases, such as rheumatoid arthritis and lupus, occur when the immune system mistakenly attacks healthy cells and tissues. The continuous immune response and chronic inflammation associated with these diseases can result in persistent fatigue and weakness.
Chronic inflammatory conditions, like inflammatory bowel disease and chronic obstructive pulmonary disease, can also cause significant fatigue due to ongoing immune activation and inflammation. The immune system’s prolonged response in these conditions can drain energy reserves and lead to a constant feeling of weakness.
On the other hand, immunodeficiency disorders weaken the immune system’s ability to fight off infections effectively. As a result, individuals with immunodeficiency disorders may experience frequent infections, which can contribute to feelings of weakness and fatigue.
Psychoneuroimmunology and Weakness
The immune system and psychological factors are intricately linked, and this interaction can influence feelings of weakness. Psychological stressors, such as chronic stress and emotional distress, can impact immune function. Prolonged stress leads to the dysregulation of the immune system, including increased production of pro-inflammatory cytokines and decreased immune cell activity.
The constant presence of these pro-inflammatory cytokines in the body can contribute to a sense of weakness and fatigue. Furthermore, poor psychological well-being, including depression and anxiety, is often associated with increased feelings of fatigue and overall decreased energy levels.
Effects of Immune System Activation on Muscle Function
Muscle weakness is a common symptom during illness or infection. The release of pro-inflammatory cytokines during immune activation can directly impair muscle function by promoting muscle breakdown and inhibiting protein synthesis. This disruption in muscle metabolism can lead to muscle fatigue and weakness.
Chronic inflammation, which can occur in conditions like rheumatoid arthritis or chronic infections, can also impact muscle strength. The systemic effects of chronic inflammation, combined with the production of pro-inflammatory cytokines, contribute to muscle wasting and decreased muscle function.
Fatigue as a Protective Mechanism
While feelings of weakness and fatigue can be unpleasant, they serve as a protective mechanism during illness. Evolutionarily, conserving energy during an infection allows the body to allocate vital resources towards mounting an effective immune response. By promoting rest and reducing physical activity, fatigue helps the body prioritize healing and recovery.
Balancing the need for rest and recovery with keeping active is crucial during periods of illness or immune activation. It is important to listen to your body and give yourself the time and rest needed for a full recovery.
Management and Support for Immune-related Weakness
Maintaining optimum immune function can help combat feelings of weakness and fatigue. Engaging in a healthy lifestyle, including regular exercise, a balanced diet, and adequate sleep, is key to supporting the immune system.
Exercise has been shown to have a positive impact on immune response and energy levels. Moderate physical activity enhances immune cell function and reduces the production of pro-inflammatory cytokines, promoting overall well-being. Additionally, eating a nutrient-rich diet, abundant in fruits, vegetables, and lean proteins, provides the necessary vitamins, minerals, and antioxidants to support immune function.
It is also important to manage stress and maintain psychological well-being. Practicing stress reduction techniques, such as mindfulness meditation or yoga, can help regulate the immune response and alleviate feelings of weakness associated with chronic stress.
In conclusion, while the immune system is crucial for protecting the body against pathogens, its activation can contribute to feelings of weakness and fatigue. Understanding the interplay between the immune system and energy balance provides insight into the mechanisms underlying these sensations. By supporting the immune system through lifestyle choices and prioritizing rest and recovery during periods of illness, you can minimize the impact of immune-related weakness and maintain overall well-being.